Global Healthcare Claims Management Market Size, Share, Trends & Growth Forecast Report By Solutions Type, Component, Delivery Mode, End-user, and Region (North America, Europe, Asia-Pacific, Latin America, Middle East and Africa), Industry Analysis From 2025 To 2033.
Global Healthcare Claims Management Market Size
The size of the global healthcare claims management market was worth USD 13.27 billion in 2024. The global market is anticipated to grow at a CAGR of 6.02% from 2025 to 2033 and be worth USD 22.46 billion by 2033 from USD 14.07 billion in 2025.
MARKET DRIVERS
Rising Health insurance in emerging countries is significantly boosting the global healthcare claims management market growth.
Health insurance is now emerging to manage people's financial needs while seeking healthcare services. Various health insurance schemes are now available on the market, with benefits ranging from a customer to an entire family. Non-life insurance firms received 17,495 crores in gross health insurance premiums between 2013 and 2014.The growing health insurance sector worldwide is expected to boost the global healthcare claims management market growth during the forecast period.
With the government shutdown and coronavirus pandemic, health insurance has created an enormous demand. According to industry researchers, previous experiences with severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS) show that demand for health insurance plans increases during epidemics, with insurers also reporting an increase in queries for pandemic coverage. Aside from increasing demand for health insurance policies, there is also an increase in demand for insurance plans with more significant sums insured. The number of people purchasing higher-sum-insured health insurance policies has risen dramatically. An increase in the number of senior citizens purchasing health insurance - Old age brings a variety of health risks and decreased susceptibility to various diseases and pandemics such as COVID-19. Immunity declines with age, making senior citizens more vulnerable to severe illnesses.The growing adoption of healthcare claims management software globally is another primary factor supporting the healthcare claims management market growth.
Healthcare claims management software is used to automate the medical claims process, improving the provider and insurance firm's relationship while shortening the patient's payment lifecycle.
These systems use automation capabilities to help hospitals and clinics fix or avoid any issues that could interrupt the claims processing and billing workflow. These systems use automation capabilities to help hospitals and clinics fix or avoid any problems interrupting the claims processing and billing workflow. Healthcare claims management software is used to automate the medical claims process, improving the provider and insurance firm's relationship while shortening the patient's payment lifecycle. Clarity's Claim Management software is a web-based application that allows joining, maintaining, and reviewing technical and general liability cases about business.Declining reimbursement rates are another considerable factor expected to accelerate the growth rate of the healthcare claims management market.
SAP has released the results of a Porter Research survey of 100 healthcare executives conducted in December 2018. According to a study, the top obstacles for health systems are declining reimbursements and patient service. The study questioned 100 healthcare executives about their organization's top concerns, 62% cited declining reimbursements, and 53% cited the patient experience. Outsourcing billing compensates for lower payment rates by the net collections after expenses. For example, for a typical three-physician practice, Software Advice estimated that outsourced billing would bring in $1,496,000 after costs, compared to just $1,241,800 for in-house billing.
Additionally, factors such as reduction in the claims denials, changes in the government services, policies, and regulations, growth in the usage of the Internet of Things (IoT) in the healthcare industry, development of Integrated Healthcare Information Systems, an aging population threatened by chronic diseases are further expected to drive the global healthcare claims management market.
MARKET RESTRAINTS
Integration of claims management systems, a shortage of qualified IT specialists in healthcare, data breaches and loss of confidentiality, risk of cyber-attack, and the high cost of deploying claims management solutions are a few of the significant restraints to the global healthcare claims management market.
Furthermore, higher incurred claims ratio, restricted product and pricing innovation, fragmented distribution of the health industry, low customer awareness, delays, and problems in health insurance claims processing and pricing limit the growth of the healthcare claims management market. The number of factors affecting claims, some of which are increasing and some of which are declining claims costs, combined with the volatility of any second wave, makes predicting experience in the short to medium term extremely difficult.
Impact Of Covid-19 On The Healthcare Claims Management Market
COVID-19 has favored the growth of the global healthcare claims management market. The COVID-19 Pandemic has negatively impacted on the global economy like no other. The COVID-19 pandemic is most likely to fuel health insurance growth in a relatively underinsured market by rising health insurance penetration. COVID-19 has a positive effect as more people want to participate in health insurance. The increase in coverage was primarily motivated by realizing that the cost of treating COVID-19 could be exceedingly high. The IRDAI (Insurance Regulatory and Development Authority of India) directive requiring insurers to provide standard coverage for COVID-19 through “Corona Kavach and Corona Rakshak Policies” also aided their cause. Given the country's low individual health insurance penetration of around 3%, COVID-19 assisted in making health insurance a priority for the average citizen. While much of the attention of insurers since the start of the COVID-19 pandemic has been on mortality and excess deaths, the crisis has also significantly impacted morbidity. Families, societies, countries, and companies of all kinds and the global economy face immense challenges due to the outbreak. COVID-19 is affecting our healthcare system and treatment procedures. Overcrowding in physicians' offices, clinics, and emergency rooms has resulted from a demand for research that must be processed elsewhere for results determinations as policymakers and regulatory agencies worldwide announced new standard operating procedures (SOPs) for industries to combat COVID-19. The pandemic has generated considerable confusion regarding determining premium rates for the next underwriting year.
REPORT COVERAGE
|
REPORT METRIC |
DETAILS |
|
Market Size Available |
2024 to 2033 |
|
Base Year |
2024 |
|
Forecast Period |
2025 to 2033 |
|
CAGR |
6.02% |
|
Segments Covered |
By Solutions Type, Component, Delivery Mode, End-user, and Region. |
|
Various Analyses Covered |
Global, Regional, and country-level analysis; Segment-Level Analysis, DROC; PESTLE Analysis; Porter’s Five Forces Analysis, Competitive Landscape; Analyst Overview of Investment Opportunities |
|
Regions Covered |
North America, Europe, APAC, Latin America, Middle East & Africa |
|
Market Leaders Profiled |
Accenture PLC, Allscripts Healthcare Solutions, Inc., Athenahealth Inc., Cerner Corporation, Genpact Limited, and Health Solutions Plus, IBM Corporation, McKesson Corporation, Optum, Inc., and Oracle Corporation., and Others. |
SEGMENTAL ANALYSIS
By Solutions Type Insights
Based on the solution type, the Integrated solutions segment is predicted to grow faster during the forecast period. Increased demand for integrated solutions, which play an important role in boosting process efficiency and lowering costs, can be attributable to this segment's rapid growth.
By Component Insights
Based on the component, healthcare claims management software is utilized to simplify the medical claims procedure, easing the connection between provider and insurance company to speed up the patient's payment lifecycle efficiently. In addition, the software segment plays a critical role in restoring people's trust. To relieve the stretched healthcare facilities across the country, epidemiological handling and preventative techniques are used with healthcare claims management software.
By Delivery Mode Insights
Based on the delivery mode, Cloud-based is the delivery mode segment that is predicted to dominate the market. Because administration and processing activities are spread across many systems, the healthcare claim management industry is complex. The claims processing rate is shorter, and administrative costs are reduced using cloud-based claim management systems. The claim administration cloud service efficiently manages all claim administrative operations, including adjudication, pricing, authorizations, and analytics. It allows for real-time claim processing with no batch processing delays. With reimbursement rates declining, healthcare providers turn to cloud-based technologies to reduce costs and ensure that insurers get paid on time. As a result of all of the above reasons, the segment is likely to develop rapidly throughout the forecast period.
By End-User Insights
Based on the end-user, the healthcare providers segment has the largest share of the market. However, the management of complicated provider networks is difficult for healthcare payers. As a result, most providers and payers in the United States depend on foreign organizations that are pioneers in claim management services.
REGIONAL ANALYSIS
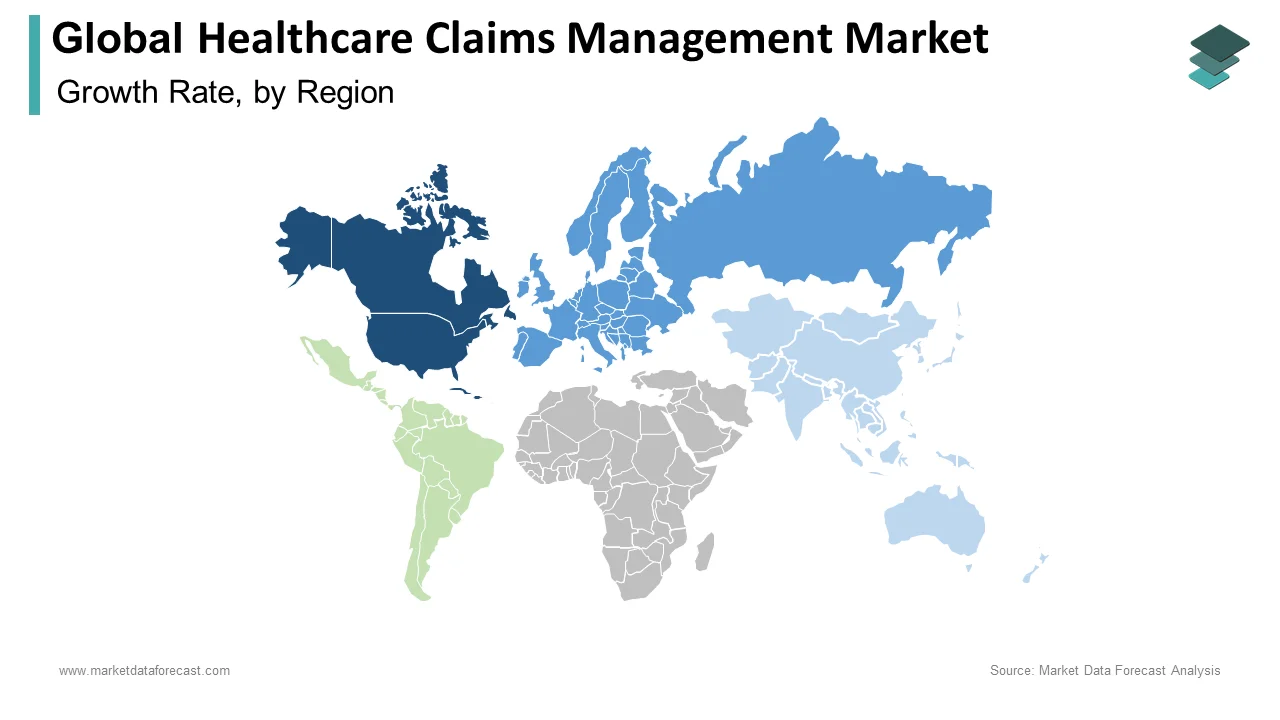
The North American market is expected to have the most significant share of the global healthcare claims management market in 2024. The high and expanding HCIT investments in the region and the presence of regulatory mandates supporting the implementation of healthcare claims management systems account for the area's large share. Most hospitals in the United States that serve Medicare or private insurance patients have difficulty processing and filing claims. As a result, accurately billing patients for a treatment or surgery is difficult for hospitals. Companies that provide healthcare claim management have a tremendous opportunity to bridge the gap. The presence of a well-established healthcare system in the region, increased insurance coverage, increased incidence of chronic diseases, and technological improvements in the sector are all contributing factors to the expansion.
Europe is predicted to maintain the second-largest share in the global healthcare claims management market. The rise in chronic illnesses, a well-established healthcare system, and increased insurance coverage drive market expansion in this region.
Asia is predicted to develop at the fastest CAGR during the forecast period. Investments to upgrade healthcare infrastructure and to expand the adoption of Healthcare IT solutions in China, steps to improve the quality of healthcare delivery in Japan, and rapid expansion of the healthcare business in India all contribute to Asia's strong growth throughout the forecast period. India and China are the key countries driving the development of the healthcare claims management software market, owing to their rapidly growing populations.
KEY MARKET PLAYERS
A few of the promising companies operating in the global healthcare claims management market profiled in this report are Accenture PLC, Allscripts Healthcare Solutions, Inc., Athenahealth Inc., Cerner Corporation, Genpact Limited, and Health Solutions Plus, IBM Corporation, McKesson Corporation, Optum, Inc., and Oracle Corporation.
MARKET SEGMENTATION
This research report on the global healthcare claims management market has been segmented and sub-segmented based on the solutions type, component, delivery mode, end-user, & region.
By Solutions Type
- Integrated Solutions
- Standalone Solutions
By Component
- Services
- Software
By Delivery Mode
- On-premises
- Cloud-Based
By End-User
- Healthcare Payers
- Healthcare Providers
- Other End Users
By Region
- North America
- Europe
- Asia-Pacific
- Latin America
- The Middle East and Africa
Frequently Asked Questions
What was the size of the healthcare claims management market worldwide in 2024?
The global healthcare claims management market was worth USD 13.27 billion in 2024.
Which segment by type held the major share of the healthcare claims management market?
The integrated solutions segment was the leader in the global healthcare claims management market in 2024.
Does this report include the impact of COVID-19 on the healthcare claims management market?
The final report includes an in-detailed analysis of how COVID-19 has changed the dynamics and growth of the healthcare claims management market.
Who are the key players in the healthcare claims management market?
Accenture PLC, Allscripts Healthcare Solutions, Inc., Athenahealth Inc., Cerner Corporation, Genpact Limited, Health Solutions Plus, IBM Corporation, McKesson Corporation, Optum, Inc., and Oracle Corporation are some of the noteworthy players in the healthcare claims management market.
Related Reports
Access the study in MULTIPLE FORMATS
Purchase options starting from $ 2500
Didn’t find what you’re looking for?
TALK TO OUR ANALYST TEAM
Need something within your budget?
NO WORRIES! WE GOT YOU COVERED!
Call us on: +1 888 702 9696 (U.S Toll Free)
Write to us: [email protected]